The COVID-19 pandemic has impacted everyone’s lives in ways we would have thought unimaginable just a few months ago. Ubiquitous stress imposed upon all age groups by the stay-at-home orders has infiltrated every household. Parents have accepted added responsibilities of schooling and working from home while sustaining a loss of income and livelihoods. Graduating seniors accepted cancellations of award ceremonies and commencement events. Students of all ages missed the camaraderie of classmates and the value of in-person interaction with their teachers. The elderly, compromised individuals, their caretakers, and frontline workers have had exceptionally difficult times. And, to all this, we have collectively adopted day-to-day lifestyle changes-- from donning masks to social distancing-- as part of our new normal.
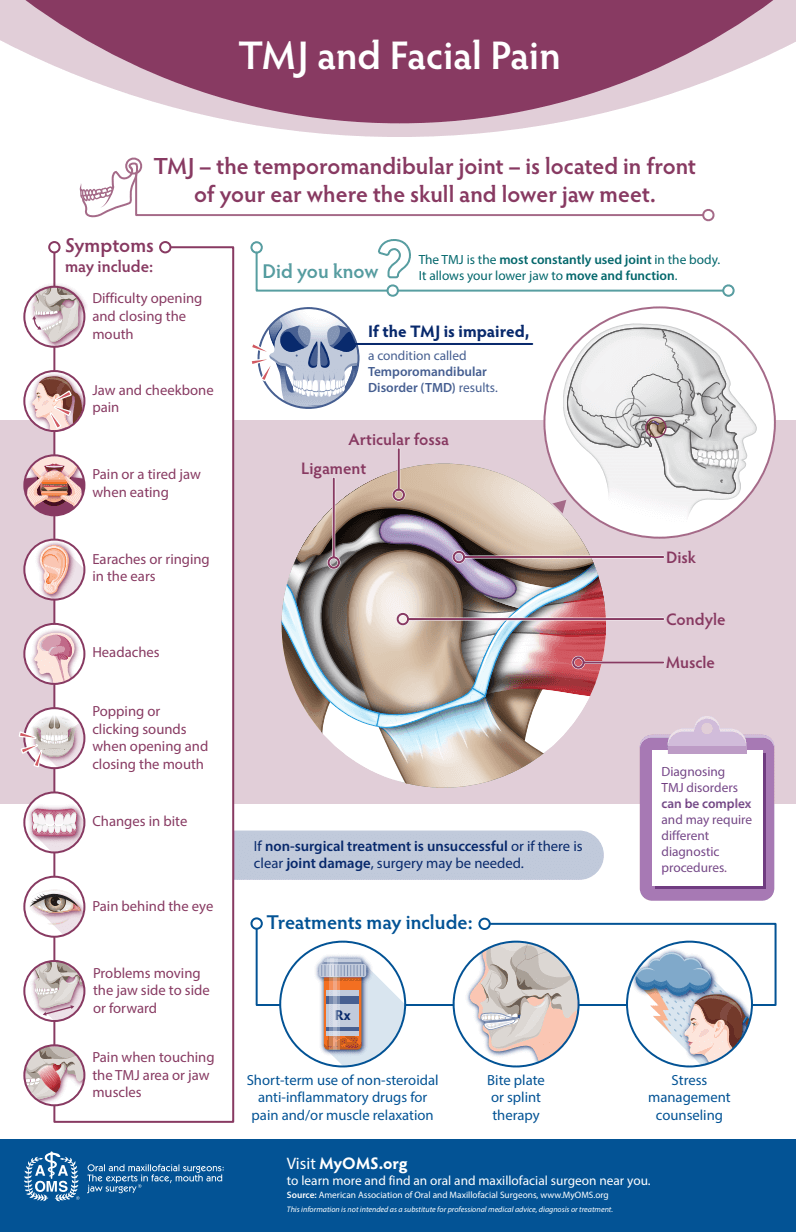
Since the start of the pandemic, and as a direct result of increased societal stressors, my oral and maxillofacial surgery practices have seen a significant increase in visits relating to pain emanating from the temporomandibular joint, commonly referred to as “TMJ”. The TMJ is located on each side of the skull in front of the ear where the lower jaw and the temporal bone meet. A small shock-absorbing disc acts as a cushion between the bones. Since it is the most active joint in the body, dysfunction of the TMJ can cause significant disruption to a person’s well-being because of the severe pain, discomfort, and functional limitations that can affect one or both sides of the face. When the TMJ is impaired, resulting symptoms are known as temporomandibular disorder or TMD. TMD is more common in women than men and among those between the ages of 20 and 40. Patients with TMD commonly report difficulty opening and closing the mouth, pain or a tired jaw when eating, pain in and around the ear that may mimic an earache, ringing in the ear, headaches, pain behind the eye, popping or clicking when opening or closing the mouth, changes in bite, and tenderness when touching the area directly in front of the ear and/or the muscles that control the jaw. While stress is a known cause of pain arising from the TMJ in response to overactive facial muscle habits like bruxism and jaw clenching, TMJ pain can also arise from misaligned or worn TMJ disc(s), arthritis, facial trauma, and pathology.
The majority of adults will experience at least one TMD related symptom in their life which, fortunately, will be mild and resolve on its own with self-managed care or non-surgical treatments. When mild symptoms do not resolve or when symptoms are moderate to severe, patients will commonly seek care at our offices where special imaging studies and diagnostic procedures will be performed. Our surgeons obtain a thorough history and clinical exam, examining the TMJ for pain, tenderness, clicking, popping, or grating noises and evaluate the way your jaw functions when opening and closing. The muscles of the face and neck are also assessed for pain and tenderness. Collectively, this information enables a proper diagnosis and, based on the diagnosis, treatment may consist of a short course of non-steroidal anti-inflammatory drugs for pain along with muscle relaxation medication, bite plate, night guard or splint therapy, and stress management counseling. Patients experiencing persistent pain or tenderness of the jaw, or are unable to open or close the jaw completely should seek consultation at our offices. Oral and maxillofacial surgeons expertly diagnose and manage hundreds of TMD patients every year. If you are experiencing temporomandibular and/or jaw muscle pain, consider consulting your general dentist or contact our specialty offices for relief of your symptoms.